The COVID-19 pandemic has been a difficult time for everyone, but for prison inmates, it has been an especially trying time. John J. Lennon is currently an inmate at Sullivan Correctional Facility in upstate New York, where he has been documenting the hardships he has been facing in prison during the pandemic. In the beginning of the pandemic in 2020, prison programs were suspended, and the prisoners were confined to their cells for all but one hour each day. Masks were not provided, resulting in 66 inmates testing positive by the end of March. It was not until the summer of 2020 when inmates began receiving a regular supply of cloth and surgical masks and hand sanitizer (Lennon).
Lennon was forced to watch his fellow inmates struggle with the worst of the virus. One inmate’s face was sunken in, was unable to breathe, and had lost weight as well as his sense of taste. Another was working out in order to gain back his strength. An older inmate has been sent to an outside hospital, as he was in need of a ventilator, and later died from the virus. Lennon himself struggled with depression and loneliness after being placed into quarantine. He notes that he missed going out to the yard to work out and talk with a friend (Lennon).
Despite the efforts to improve sanitation inside of prisons, prisoners are being infected and dying at higher rates compared to the general population, with prisoners testing positive at four times the rate of the general population and dying at twice the outside rate, both as of only December 2020 (Lennon). It is clear that COVID-19 thrived in the prison system, but why did this happen, and how can we prevent it in the future?
Prisons and Pandemics Throughout History
Historically, pandemics tend to surge through the prison system in the United States, with just some examples explored below.
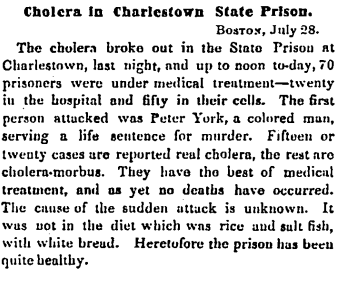
Cholera
In 1854, the United States experienced an outbreak of cholera, a disease causing diarrhea and a ghostlike appearance (McMillen 60). The Charlestown State Prison experienced an unexpected increase in cases for an unknown reason. In under 24 hours, 70 prisoners were being treated for the disease (“Cholera in Charlestown State Prison”). One contracts cholera from ingesting contaminated water, so it is likely that the Charlestown inmates were expelling contaminated waste that was essentially poisoning their drinking water due to the poor sanitary conditions in prisons.
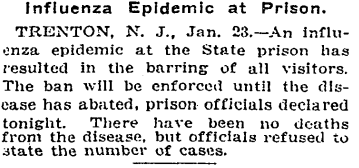
Influenza
The 1920 Influenza outbreak also affected prisons in similar ways to the COVID-19 pandemic. As with the coronavirus, influenza symptoms include cough, fever, chills, fatigue, sore throat, and runny nose (Crosby 5). Additionally, the two spread the same way- through droplets released when coughing, sneezing, or talking- which aided in both viruses’ spread throughout the prison systems. During the 1920 Influenza outbreak, the New Jersey State Prison experienced a sudden increase in influenza cases, causing the prison to close to any visitors (“Influenza Epidemic at Prison”). This is similar to today’s COVID-19 pandemic, as the prison closed to visitors, suspended programs, and banned movement within the facility.
AIDS
The 2001 AIDS epidemic not only affected its most common target- gay men and drug users- but also prisoners. During this time, tens of thousands of inmates were affected, as the behaviors that spread the disease (sex or sharing needles) are common in prisons. Additionally, the necessary precautions, such as condoms and sanitary products, are unavailable to prisoners (“AIDS in Prisons”). This is similar to the COVID-19 pandemic, as the necessary sanitary products, such as masks and hand sanitizer, were widely unavailable to prisoners. These various instances show how easily diseases spread throughout the prison system. Given the years of experience, why weren’t prison officials and the government more prepared to handle COVID-19 and stop the spread more efficiently?
Prisons and COVID-19
Prisons all across the country experienced COVID-19 outbreaks due to their lack of preparation and failure to follow the necessary precautions. At first, many facilities focused on keeping the virus out, instead of preparing for once it reached the inside of the facility. Additionally, some did not follow sanitary guidelines, including failure to supply soap, test inmates being transferred between facilities, and enforcing masks. Testing was slow for both inmates and prison employees, who were also not contact traced quick enough. Finally, prisons operate over capacity, allowing for the virus to spread quickly and easily, as social distancing is not possible (Burkhalter et al.). All of these mistakes caused detrimental effects. In prisons, 34 in 100 inmates have COVID, while only 9 in 100 people in the entire United States have the virus. In this past year, 1,400 new cases and seven deaths average daily in prisons (Burkhalter et al.).
Stopping the Spread
Some organizations have taken matters into their own hands and worked to help prisons become a more COVID-safe environment. Amend at the University of California San Francisco developed guidelines and training on masks, sanitation, and social distancing for prison staff and inmates. They also worked to get more testing opportunities and improve the available healthcare for prisoners (Kurtzman). These efforts started after the pandemic had already begun affecting so many lives. If these programs and precautions were already in place, it is likely that less lives would have been affected by COVID-19.
The Future of the Prison System
Given our nation’s history with pandemics thriving within our prison systems, it is my hope that we can work towards creating a more sanitary environment for our prisons. This can be done by working towards ending overcrowding and continuing to provide the necessary safety and sanitary precautions. In doing so, any future outbreaks can be contained quickly and easily so that less lives are affected, both inside and outside of the prison.
Works Cited
“AIDS in Prisons.” New York Times (1923-Current file), May 21, 2001, pp. 1. ProQuest, http://unh-proxy01.newhaven.edu:2048/login?url=https://www-proquest-com.unh-proxy01.newhaven.edu/historical-newspapers/aids-prisons/docview/92062557/se-2?accountid=8117.
Burkhalter, Eddie, et al. “Incarcerated and Infected: How the Virus Tore Through the U.S. Prison System.” The New York Times, 10 Apr. 2021, www.nytimes.com/interactive/2021/04/10/us/covid-prison-outbreak.html.
“Cholera in Charlestown State Prison.” Hartford Daily Courant (1840-1887), Jul 29, 1854, pp. 2. ProQuest, http://unh-proxy01.newhaven.edu:2048/login?url=https://www-proquest-com.unh-proxy01.newhaven.edu/historical-newspapers/cholera-charlestown-state-prison/docview/553084527/se-2?accountid=8117.
Crosby, Alfred W. America’s Forgotten Pandemic: The Influenza of 1918. 2nd ed., Cambridge University Press, 2010.
“Influenza Epidemic at Prison.” New York Times (1857-1922), Jan 24, 1920, pp. 4. ProQuest, http://unh-proxy01.newhaven.edu:2048/login?url=https://www-proquest-com.unh-proxy01.newhaven.edu/historical-newspapers/influenza-epidemic-at-prison/docview/98244224/se-2?accountid=8117.
Kurtzman, Laura. “For Prisoners, Pandemic Hits with Greater Force.” University of California San Francisco, 25 Oct. 2020, www.ucsf.edu/news/2020/10/418876/prisoners-pandemic-hits-greater-force.
Lennon, John J. “I’m Incarcerated. This Is My Covid Lockdown Story.” The New York Times, The New York Times, 6 Apr. 2021, www.nytimes.com/2021/04/06/magazine/prison-covid.html?auth=login-email&login=email.
McMillen, Christian W. Pandemics: A Very Short Introduction. Oxford University Press, 2016.


Interesting how similar these outbreaks are even though they span 100 years. Technology is obviously a factor. Prisoners also should’ve been offered vaccines much sooner to help stop the spread